Hello everyone,
Another week has passed us by. We officially hit 4 months post op, which is a big deal in this house, because it means I could walk the dogs again. I was happy to have my walking buddies again, Finley and Gracie were happy to go, although they seem to have forgotten their walking manners, and Mom was happy because we tired them out and they weren’t so naughty. Not lifting, pushing or pulling more than 30 pounds for 4 months is trickier than you think. Keep on healing ol’ sternum.
If you didn’t see my facebook post earlier this week, the title of this post will make no sense. Dr. Pepper took Caffeine Free Diet Dr. Pepper out of production and I nearly had a meltdown over it. I don’t drink, I don’t smoke, but I love a fountain drink or a diet dr. pepper. Its like my little treat. Only problem is that since transplant and with all my meds, especially steroids, my body can’t handle caffeine, so enter caffeine free Diet Dr Pepper. Well, I went to order it, after a frustrating appointment and a morning dealing with insurance companies and it could no longer be found. I nearly broke down at the kitchen table. I think my direct quote was “you’ve got to be kidding me..this is so not my day”.
It was never about the diet dr pepper. It was about disappointment. I can laugh about it now, but it was like the straw that broke the camels back.
I shared last week about my Blood Pressure being high. Well that darn blood pressure is being so stubborn, that we had to add a second medication to manage it and have already had to double the dose. I am disappointed that we had to add another medication to manage it. My body does not like medication changes, so for a few days after we make one, I feel pretty crummy.
I saw my PCP in person this week for the first time in 10 months. I see her via telemedicine every two weeks, but she wanted to evaluate me in person and since I have the covid antibodies, we decided now would be the time to do it, minimizing risk. Why in person? Well, I have been complaining to the transplant team that I was having a lot of neck, back and left shoulder pain. They kept saying “we will watch it”, but I could tell something was off. I didn’t have this pain after the first open heart surgery and it was getting worse and my shoulder felt almost locked. Well, after a very disappointing (catching a theme for today?) appt with my general cardiologist about two weeks ago, I emailed him to followup on medications and the blood pressure and I explained to him that I thought the hypertension was multifaceted, including because I was in a lot of pain. When he was speaking to my PCP last week via phone about my blood pressure he asked her about it and expressed concern that the pain and so they agreed my PCP would evaluate.
Turns out….I have what is known as frozen shoulder and I am in the freezing stage. Frozen shoulder is just that, your shoulder becomes locked or frozen and during the freezing stage you are in the pain stage as you slowly lose range of motion. Then it goes into the frozen stage where you are stuck at that loss of range of motion and then eventually it will thaw/heal. Guess how long it can freeze for…up to or more than a year. When she told me, I started laughing. It was either that or tears.
What can we do about it? Not much, we can’t use the typical medication treatments like NSAIDs due to my transplant/other meds, physical therapy is out because of covid/post transplant and injecting steroids would only provide a temporary relief but throw my body all out of whack, so the risk outweighs the benefit. So what are we doing? Heating pads, lidocaine patches and a topical steroid and stretching as tolerated. My PCP did warn me that the pain is likely to get worse and some people do require pain medication if it becomes unbearable or if it continues to wake me up.
So how’d I get frozen shoulder? Women and diabetics are more prone and my elevated blood sugars from steroids likely didn’t help. It can also be due to immobility, so during the post-op period when I was protecting the upper body from pain, I wasn’t using the arm as much, the perfect storm happened and now I have a frozen shoulder. We did do an x-ray just to be sure, as steroids can affect the joints, but it would be pretty early on for that to happen, so we don’t expect the x-ray will find anything.
To say I’m disappointed to have another pain issue thats only complicated by the fact that we can’t properly treat it due to the surgery we did to get rid of another chronic pain, would be pretty accurate. The fact that it was dismissed at Hopkins because they thought it was ‘memory pain or in my head’ (thanks, ID) and not evaluated, is disappointing.
My PCP said something very insightful yesterday, ‘don’t punish yourself for the past’. I downplayed the pain and stopped reporting it, because I just didn’t have the fight in me to go toe to toe with providers again. I knew exactly where the conversation would go, because its already gone there multiple times since transplant…”you are too young, are you sure you aren’t just remembering your past pain, we don’t know the source of your pain so we don’t think you have it, are you sure we don’t just need to bring in psych?”. You guys, I had a transplant due to chronic chest pain and I still get questioned about if my pain is real, have to argue that I am not a drug-seeker and its still a fight. Major disappointment.
There were a lot of other disappointments this week. My labs resulted and they were off again. My WBC is 2.1, which is super low, which means I have to give myself an injection to stimulate bone marrow and make white blood cells. It causes excruciating bone pain and the last time I had to do it I got sick because the pain was so severe. We also have to had to hold a few anti-rejection meds until it rebounds, which no one loves, including myself. My kidneys also are also getting cranky again so I have to get labs redrawn on Monday. At this point, normally we would be to labs every 3/4 weeks but unfortunately these lab results mean we are back to weekly labs for a while.
I thought you just had perfect labs? I did. This is the reality of being immune compromised and all the transplant meds. We also are increasing and maxing out doses of meds that can affect the kidneys, so we expected some change, just not this much. This week we are also adding another anti-viral medication as a preventative, per Transplant IDs suggestion. We’ve made 4 med changes this week alone and likely more next week. From a cardiac perspective, things continue to improve, we just have a lot of work to do to get the rest of my body to fall in line.
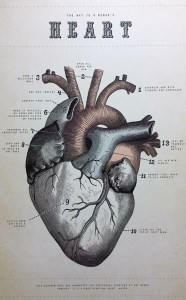
We head back to the Cath lab the second week of February for the next Cath/Biopsy/echo and hopefully it will continue to show good results. We also are a few days short of the two week countdown to February 5th. Its a big day in this house this year: my trusty sidekick’s birthday and National Wear Red Day to raise awareness for heart disease. So if you don’t have any red, heres an excuse to do some online shopping or rock your “Hope Wins” items on that day.
I know that this post isn’t the most uplifting post, but I have always promised to be truthful on this blog and it was a disappointing week in many ways. Do I lose my you know what over it sometimes? Yep. Do I get cranky about it sometimes? Just ask Mom. Did I emotionally eat some ice cream over the weekend. Sure did. Do I laugh about it? Yes, eventually….so long diet dr pepper. Do I believe things will get better? 100%…because Hope wins.
Am I thankful for the opportunity to have good days and bad because of the gift of a donor and their family? 100% of the time. They are the true heroes of this story.
See you for the next update. Love, K